In the mid-20th century, anabolic steroids were hailed as a medical breakthrough. Doctors and scientists hoped these synthetic hormones could treat muscle-wasting illnesses, aid recovery from trauma, and promote healthy growth. Early on, results looked promising – patients showed improved appetite, weight gain, and muscle mass. Yet by the 1960s, the shine had worn off. The medical use of steroids was revealing serious drawbacks.
This article examines the early enthusiasm for anabolic steroids in the 1940s–50s, the major limitations that emerged in practice, the specific side effects that derailed their medical potential, and how these failures led to the development of Selective Androgen Receptor Modulators (SARMs) as a safer alternative.
Initial Medical Enthusiasm for Anabolic Steroids (1940s–1950s)

In the 1940s and 1950s, testosterone derivatives burst onto the scene with great medical fanfare. Researchers had discovered testosterone (the primary male hormone) in the 1930s and soon began modifying its structure to create synthetic anabolic steroids that could boost strength and tissue growth.
The goal was to harness testosterone’s anabolic effects (muscle and bone building) while minimizing its masculinizing (androgenic) effects. Early laboratory and clinical reports were encouraging – these synthetic hormones appeared to help patients regain weight after severe illnesses, heal faster from injuries, and combat chronic fatigue.
Doctors reported cases of improved nitrogen retention (a sign of muscle growth) and better recovery in malnourished or post-surgical patients. There was a prevailing optimism that anabolic steroids could become “miracle drugs” for a range of conditions from muscle wasting diseases to osteoporosis.
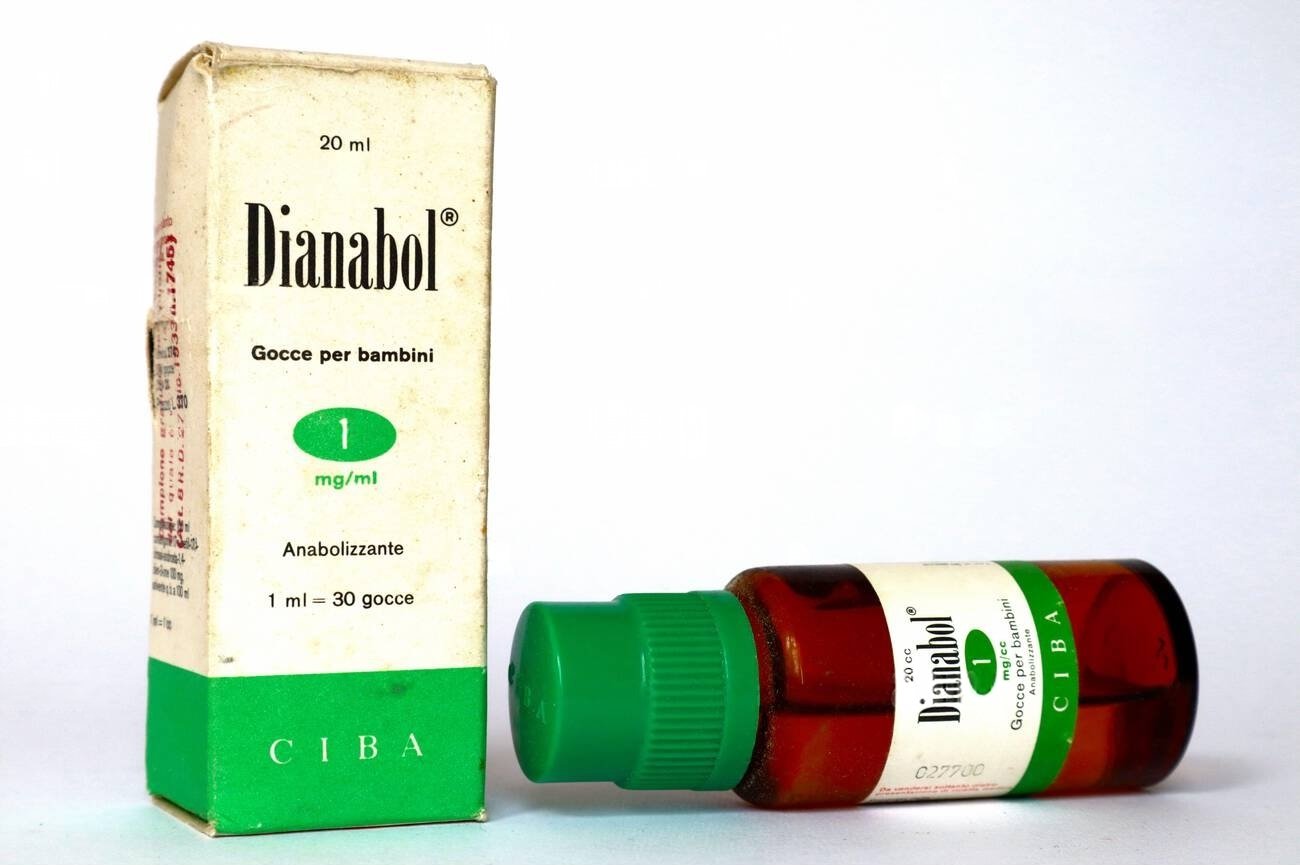
One landmark event symbolizing this early optimism was the development of methandrostenolone (Dianabol) in 1958. Dianabol was an orally active steroid created by Dr. John Ziegler and colleagues, intended to provide the muscle-building benefits of testosterone in a convenient pill. It quickly proved effective at enhancing protein synthesis and lean body mass – athletes and patients alike experienced rapid muscle gains.
Early clinical reports and anecdotal successes rolled in: burn victims and bedridden patients given anabolic steroids seemed to recover faster, and underweight individuals gained strength. Such results fueled hopes that these drugs could revolutionize medicine.

By the late 1950s, anabolic steroids were being prescribed for anemia, severe infections, trauma recovery, and even to frail elderly patients, all under the belief that these “targeted hormone therapies” could rebuild a healthier body. The steroid era had begun on a hopeful note, with many in the medical community convinced they had found a powerful new therapeutic tool.
Major Limitations Revealed in Clinical Practice
However, as doctors broadened the medical use of steroids, significant limitations and side effects began to surface. The early enthusiasm gave way to clinical reality: these drugs were far from the risk-free panacea imagined. Two major problems became evident:
- Lack of Tissue Selectivity: Anabolic steroids turned out to be blunt instruments. They lacked the ability to target only muscle and bone. In practice, administering testosterone or its analogs “bathed” the entire body in androgenic stimulation. Every tissue with androgen receptors – the prostate, liver, skin, etc. – would respond, not just muscles. This meant patients experienced unwanted androgenic activity alongside the desired anabolic effects.
For example, women treated with early steroids for anemia soon showed masculine traits (virilization), such as facial hair growth and a deeper voice, due to stimulation of hair follicles and vocal cords. Men on high doses would see their testes shrink as natural testosterone production was suppressed.
No matter how chemists tweaked the molecule, none of the early anabolic steroids could completely separate anabolic and androgenic effects – a fact underscored by rat experiments in the 1950s showing that all tested compounds still enlarged the prostate (an androgen-sensitive organ) while building muscle. This lack of selectivity severely limited safe usage. - Hormonal Side Effects and Liver Toxicity: It also became clear that anabolic steroids carried a host of systemic side effects. Hormonal side effects were especially problematic. Because these drugs flood the body with androgens, the endocrine system’s feedback loops go awry. Men could develop breast tissue (gynecomastia) from excess testosterone converting to estrogen, and women could experience menstrual disruptions and infertility.
Almost all patients on long-term steroids showed changes in cholesterol levels, blood pressure, or liver enzymes. In fact, by the 1960s doctors recognized a specific form of liver damage caused by oral anabolic steroids: cholestatic liver toxicity. To make steroids pill-friendly, chemists 17α-alkylated the testosterone molecule – a modification that survived liver metabolism. Unfortunately, this change was a double-edged sword.
Patients taking 17α-alkylated oral steroids (like methyltestosterone or Dianabol) sometimes developed jaundice and liver dysfunction due to cholestasis (bile back-up) or even rare liver tumors. Unfavorable cholesterol changes were another issue – steroids tended to lower HDL (“good” cholesterol) and raise LDL (“bad” cholesterol), potentially elevating cardiovascular risk. These side effects might be acceptable in a short-term emergency treatment, but for chronic use they were untenable.
By the end of the 1960s, the medical community realized that their anabolic wonder drugs were a double-edged sword. Testosterone’s molecular structure (shown above) allowed it to interact with receptors all over the body, and simply modifying the molecule slightly could not eliminate this broad action. As one research review noted, “Adverse side effects of AAS include sexual dysfunction, alterations of the cardiovascular system, psyche and behavior, and liver toxicity.” In other words, patients often paid a price for the muscle gains.

Testosterone itself was also impractical as a long-term medication: it had to be injected or given as implants, since oral dosing didn’t work (unmodified testosterone is destroyed by the liver). The oral analogs that were developed solved the delivery issue but caused new problems like liver strain.
Moreover, these drugs were not suitable for women or children – giving an adolescent boy or a woman an anabolic steroid might strengthen muscle, but it would almost certainly cause virilization or stunt growth by fusing bone growth plates prematurely. Thus, for all their initial promise, anabolic steroids proved to be blunt, risky medications.
The early steroid era taught scientists and clinicians two key lessons: (1) tissue selectivity – the dream of isolating muscle-building effects – was highly desirable but nearly impossible with the steroid chemistry of the time; and (2) any future solution would require a radically different approach to avoid the widespread side effects.
Specific Reasons Why Anabolic Steroids Fell Short
Digging deeper into the medical literature of the 1950s–1970s, several specific reasons emerge for why anabolic steroids failed to meet expectations as long-term therapies:
- Androgenic Side Effects in Women: Perhaps the clearest limitation was in female patients. Early trials of anabolic steroids in women (for conditions like advanced breast cancer or severe osteoporosis) had to be halted due to virilizing side effects. Even at moderate doses, women developed male-pattern hair growth, acne, voice deepening, and clitoral enlargement. These changes were often irreversible and obviously unacceptable for routine treatment. This meant half the patient population (women) essentially could not use anabolic steroids for most indications – a huge medical limitation.
- Hormone Suppression in Men: Paradoxically, giving exogenous testosterone analogues suppressed the body’s own hormone production. Male patients on steroids would experience hypogonadism – the testes shut down testosterone and sperm production via negative feedback to the pituitary. Medically, this led to testicular atrophy and infertility in men, especially with long-term use. Doctors found that once an anabolic steroid was discontinued, it could take months for normal hormonal function to recover. This suppression was a serious drawback for treating young men, who might end up with the very hormone imbalances the therapy was supposed to fix.
- Liver Damage with Oral Steroids: As mentioned, the 17α-alkylated oral steroids (e.g. methyltestosterone, stanozolol, oxymetholone) caused particular concern. Cases of drug-induced hepatitis and benign liver tumors were documented in patients on long-term oral anabolic steroids. One classic report from the 1960s described patients who developed peliosis hepatis (blood-filled cysts in the liver) after extended steroid use. Because many of the conditions doctors hoped to treat (like chronic lung disease or dialysis-related wasting) would require months or years of therapy, this liver toxicity made anabolic steroids a non-starter for those purposes.
- Cardiovascular Risks: Over time, physicians also observed that anabolic steroids could negatively affect the heart and blood vessels. Patients on steroids sometimes showed high blood pressure, left ventricular hypertrophy, and cholesterol disturbances. While these effects were more thoroughly documented in the bodybuilding community (where doses were very high), even therapeutic doses raised concern about accelerating atherosclerosis or causing arrhythmias in susceptible individuals. The long-term medical use of steroids to improve physical function had to be weighed against a potential increase in heart disease risk, a calculus that often came out unfavorable.
- Behavioral and Other Effects: Some patients on anabolic steroids reported mood swings, increased aggression or irritability (so-called “roid rage”), or other psychological effects. Although difficult to quantify, these neuropsychiatric side effects further tarnished steroids’ profile as a safe chronic medication. Additionally, anabolic steroids could cause minor but disruptive side effects like acne flares, oily skin, and in men, breast tissue enlargement due to estrogen conversion. In children and adolescents, as noted, steroids could prematurely stop bone growth, leading to short stature. All of these issues, while tolerable in a short-term emergency use, became unacceptable in long-term therapy.
In summary, by the 1970s the consensus was that anabolic steroids fell short of medical expectations. They were certainly powerful at building muscle and had legitimate uses (for example, in treating delayed puberty or certain anemias), but their pharmacological limitations – lack of selectivity and organ toxicity – meant they could not be widely applied to chronic conditions.
As one review noted, serious adverse effects tended to appear “following prolonged use of AAS at high dose”, which is exactly what long-term medical treatment would entail. Thus, clinicians largely restricted anabolic steroids to narrow uses (such as testosterone replacement in male hypogonadism) and looked for alternative strategies for other patients. It was this disappointment that directly spurred scientists to find a better solution.
How Medical Failures Led to the Development of SARMs
The failure of early anabolic steroids to provide safe, selective therapy did not mark the end of the anabolic dream. Instead, it prompted a new wave of research to “have our cake and eat it too” – to separate anabolic benefits from side effects. Pharmacologists in the 1980s and 1990s, armed with a growing understanding of hormone receptors, began pursuing a novel idea: Selective Androgen Receptor Modulators. The concept was inspired in part by the success of selective estrogen modulators (like tamoxifen), which could block estrogen’s effects in the breast while mimicking estrogen in bone. If something similar could be done for the androgen (testosterone) pathway, it could revolutionize therapy.

Researchers reasoned that the problem with steroids wasn’t that anabolic effects were impossible to achieve – it was that the delivery method was too indiscriminate. The key would be to design molecules that target the androgen receptor (AR) in a tissue-selective way. In the late 1990s, this vision became a reality. For the first time, scientists discovered non-steroidal molecules that could bind and activate the AR in muscle and bone, but had significantly less effect on other tissues.
These compounds were chemically very different from testosterone (they weren’t based on the four-ring steroid structure at all). As a result, they did not get converted to estrogen or DHT – meaning no inadvertent breast tissue growth or prostate overstimulation. Early candidates like ostarine (enobosarm) and LGD-4033 showed they could increase lean muscle mass in clinical trials without the dangerous liver impact of 17α-alkylated steroids and with much milder testosterone suppression.
Dr. James Dalton and Dr. G. Negro-Vilar were among the pioneers who championed these compounds in 1998–1999, coining the term “Selective Androgen Receptor Modulators” or SARMs. They envisioned SARMs as “anabolic steroids with brainier control mechanisms”, essentially delivering the muscle and bone benefits without the baggage. The SARMs benefits quickly became evident in research: they were orally active (like steroids) but organ-selective (unlike steroids).
Studies showed SARMs could increase muscle and bone density in animal models while sparing the prostate and other organs. Importantly, they did not cause the cholestatic liver damage associated with steroid pills and did not significantly shrink the testes at moderate doses (any suppression of hormones was reversible upon stopping the drug). For women, SARMs offered a potential anabolic therapy that wouldn’t cause virilization, since the compounds were selective enough to avoid triggering the full spectrum of male secondary sexual characteristics.

It’s worth noting that SARMs are not themselves “steroids” in the chemical sense. In popular conversation, some people refer to them as “SARMs steroids,” but this is a misnomer. They are better described as SARMs: steroid alternatives. Whereas anabolic steroids are variations of the testosterone molecule, SARMs are a different class entirely – often aryl-propionamides, hydantoins, or other novel scaffolds. This fundamental difference is why SARMs side effects thus far appear more benign.
For example, testosterone can convert to estrogen (causing breast tissue growth in men) and DHT (fueling prostate growth and hair loss), but SARMs cannot undergo those conversions. That said, SARMs are not side-effect free – they can still cause some suppression of natural testosterone and mild liver enzyme changes in certain cases. But compared to anabolic steroids, the risk profile is significantly improved, and no severe organ toxicities have emerged in short-term studies.

In essence, the drive toward SARMs was a direct response to the shortcomings of anabolic steroids. Decades of research and disappointment taught scientists what the “ideal” anabolic therapy should look like: an orally available compound that builds muscle and bone without affecting the prostate, skin, or liver. SARMs were designed to meet these criteria. Early trials in humans have validated many of these points – showing increases in lean body mass with minimal androgenic side effects.
As of today, SARMs remain investigational (none are yet approved for general medical use), but they represent the fulfillment of a vision that arose directly from the steroid era’s failures. Researchers often describe SARMs as “the best of both worlds,” aiming to finally achieve what those early steroid researchers in the 1940s and 50s had hoped for: targeted anabolic therapy that can truly help patients without doing harm.
FAQs
Why did doctors initially think anabolic steroids would revolutionize medicine?
Doctors initially believed anabolic steroids could transform medicine because they rapidly increased muscle mass, stimulated weight gain, and improved recovery in patients suffering from severe illness, trauma, and muscle-wasting conditions. Early clinical successes in the 1940s and 1950s, like faster healing after surgery and improved strength in malnourished patients, fueled optimism about their widespread medical potential.
What specific medical issues caused anabolic steroids to fall out of favor?
Anabolic steroids fell out of favor due to serious medical issues such as liver damage, hormonal disruptions, and cardiovascular risks. Liver toxicity, particularly from oral steroids, led to conditions like jaundice and liver tumors. Patients also experienced androgenic side effects like masculinization in women and testicular shrinkage in men, making long-term medical use unsustainable.
How did problems with anabolic steroids inspire the creation of SARMs?
The medical failures of anabolic steroids, particularly their inability to selectively target muscle without harmful side effects, directly inspired scientists to develop SARMs. Researchers aimed to create compounds that selectively activated muscle and bone growth while minimizing hormonal disturbances and liver toxicity, addressing the exact shortcomings steroids presented.
Were anabolic steroids ever successfully used medically despite their limitations?
Yes, anabolic steroids did find limited medical success for short-term use, such as treating severe anemia, assisting recovery from serious trauma or burns, and providing hormonal replacement in conditions like delayed puberty or hypogonadism. However, their adverse side effects significantly restricted their long-term medical application.
Do SARMs completely eliminate the side effects seen with anabolic steroids?
SARMs significantly reduce, but do not completely eliminate, the side effects observed with anabolic steroids. They offer improved selectivity, meaning they typically avoid issues like liver damage, severe masculinization, or excessive prostate growth. However, SARMs may still cause mild testosterone suppression or mild cholesterol changes, requiring careful medical supervision.
Conclusion
The early enthusiasm surrounding anabolic steroids in medicine quickly turned to disappointment as clinicians confronted their serious limitations. While initially hailed as revolutionary treatments, steroids revealed significant issues: lack of tissue selectivity, substantial hormonal disruptions, and severe liver toxicity – that rendered their long-term medical application unfeasible. This stark realization drove researchers toward innovative solutions, ultimately leading to the invention of Selective Androgen Receptor Modulators (SARMs).
Unlike steroids, SARMs promised the targeted muscle-building benefits that medical science originally sought, without the dangerous side effects that undermined steroid therapy. Today, understanding why anabolic steroids failed helps us appreciate the critical need for ongoing research into SARMs and similar targeted therapies. Those interested in the future of muscle-wasting treatments and safer hormone therapies are encouraged to continue exploring SARMs, as these innovative compounds strive to deliver what anabolic steroids could not – effective medical benefits with significantly fewer risks.
References
- Hoffman, J. R., & Ratamess, N. A. (2006). Medical issues associated with anabolic steroid use: Are they exaggerated? Journal of Sports Science & Medicine, 5(2), 182–193. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3827559/
- National Institute on Drug Abuse (NIDA). (2006). Research report series: Anabolic steroid abuse. Retrieved from https://nida.nih.gov/sites/default/files/rrsteroids_0.pdf
- National Institutes of Health (NIH). (2018). Androgenic steroids. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK548931/
- Solimini, R., Rotolo, M. C., Mastrobattista, L., Mortali, C., Minutillo, A., & Pacifici, R. (2017). Anabolic androgenic steroids and hepatotoxicity: A brief review. Annali dell’Istituto Superiore di Sanità, 53(2), 169–175. https://doi.org/10.4415/ANN_17_02_12. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9331524/
- Koller, T., & Negro-Vilar, A. (1999). Selective androgen receptor modulators (SARMs): A novel approach to androgen therapy for the new millennium. Journal of Clinical Endocrinology & Metabolism, 84(10), 3459–3462. https://doi.org/10.1210/jcem.84.10.6070. Retrieved from https://journals.sagepub.com/doi/full/10.1621/nrs.06010
- Mohler, M. L., Bohl, C. E., Jones, A., Coss, C. C., Narayanan, R., & Dalton, J. T. (2009). Nonsteroidal selective androgen receptor modulators (SARMs): Dissociating the anabolic and androgenic activities of the androgen receptor for therapeutic benefit. Journal of Medicinal Chemistry, 52(12), 3597–3617. https://doi.org/10.1021/jm900280m. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5595949/
- Bhasin, S., & Jasuja, R. (2009). Selective androgen receptor modulators (SARMs) as function promoting therapies. Current Opinion in Clinical Nutrition and Metabolic Care, 12(3), 232–240. https://doi.org/10.1097/MCO.0b013e32832a3d79. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5896569/
- Kanayama, G., Hudson, J. I., & Pope Jr, H. G. (2008). Anabolic-androgenic steroid abuse: Psychiatric and physical costs. Cleveland Clinic Journal of Medicine, 75(5), 341–352. https://doi.org/10.3949/ccjm.75.5.341. Retrieved from https://www.ccjm.org/content/ccjom/74/5/341.full.pdf
- Chowdhury, A., Ahmed, I., Alharthi, R., & Alam, F. (2022). Anabolic steroid-induced cholestatic liver injury: A case report. Cureus, 14(8), e27638. https://doi.org/10.7759/cureus.27638. Retrieved from https://www.cureus.com/articles/100856-anabolic-steroid-induced-cholestatic-liver-injury-a-case-report.pdf
About the author

Emiliano Ventura, PhD, Pharm.D.
Senior Scientist MetID & LC-MS
🧑🔬 Senior Scientist | 🧪 Bioanalytical Methods (LC-MS/MS) | 🔍 MetID (HRMS, Radiodetection) | 💊 Small Molecules 🧱 Peptides 🧬 Oligonucleotides | 🚴 Anti-Doping | 🌍 Life Sciences | 🌟 Science with Purpose
Find me on LinkedIn!
Read more
Explore the Historical Development of SARMs in our series of articles:
Early Anabolic Steroid Era (1940s–1960s):
1. How the First Anabolic Steroids Were Created
2. Why Early Anabolic Steroids Fell Short of Medical Expectations
3. Hershberger Test: How Scientists Measured Anabolic vs Androgenic Effects
Discovery of Hormone Receptors (1960s–1970s)
1. How Discovery of Androgen Receptors Changed Hormone Therapy
2. Role of Nonsteroidal Antiandrogens in SARMs Development
3. The Crucial Difference Between Steroidal and Nonsteroidal Androgens
Concept of Selective Receptor Modulators (1980s)
1. The Revolutionary Concept Behind SERMs
2. Why SERMs Became a Blueprint for SARMs
3. How Tissue Selectivity Became the Core of Hormonal Drug Development
The Birth of SARMs (1990s)
1. The Story Behind the First Nonsteroidal Androgen Receptor Agonists
2. James Dalton’s Groundbreaking Research on SARMs
3. Early SARMs Structures and Their Advantages Over Steroids
Rapid SARMs Expansion (2000s)
1. Early Human Trials of Ostarine: Promises and Results
2. Ligandrol (LGD-4033): A Powerful SARM in Clinical Research
3. Chemical Diversity of SARMs Developed in the 2000s
Clinical Trials and Regulatory Challenges (2010s)
1. Phase III Clinical Trials of Ostarine: Successes and Failures
2. Why Defining Clinical Endpoints Was Difficult for SARMs Trials
3. Regulatory Hurdles Facing SARMs Approval
SARMs in Sports and the Rise of Misuse
1. How SARMs Became the New Doping Trend in Sports
2. Why Athletes Were Attracted to SARMs Despite Risks
3. Health Consequences of Illegal SARMs Use: Documented Cases
SARMs Today and Future Perspectives (2020s)
1. Current SARMs Research: Where Do We Stand?
2. Potential Medical Applications of SARMs in the Next Decade
3. Emerging Compounds and Future Directions in SARMs Research
