The Hershberger test is a classic in vivo bioassay that allows researchers to quantify a compound’s anabolic activity relative to its androgenic effects. Developed in the mid-20th century to screen anabolic steroids, this assay measures muscle growth versus male reproductive organ growth in castrated rats. It remains a cornerstone method in pharmacology for evaluating how strongly a substance stimulates muscle development (anabolic effects) compared to male sex tissues (androgenic effects).
What is the Hershberger Test?
The Hershberger test (or Hershberger assay) is an in vivo scientific methodology used to detect androgenic and anabolic effects of substances in male rats. It was first described in 1953 by Dr. T. V. Hershberger and colleagues as a way to differentiate a compound’s muscle-building capability from its masculinizing side effects.
In this test, researchers use castrated male rats (which lack endogenous testosterone) and administer a test compound to see if it can regrow certain tissues. By the 1950s, the assay became a crucial tool in steroid research, helping scientists screen new anabolic steroids for a better androgenic–anabolic ratio. A compound that significantly increases muscle size but causes minimal prostate growth would show high anabolic selectivity.

Historical context: At the time, anabolic steroid developers were seeking drugs that could promote muscle growth for medical use without severe male hormone side effects. The Hershberger assay provided a quantitative measure: if a novel steroid made the rat’s levator ani muscle (a pelvic muscle very sensitive to androgens) grow larger, it indicated anabolic activity, whereas enlargement of the prostate and seminal vesicles indicated androgenic effects.

This allowed researchers to rank compounds by their androgenic-anabolic ratio. The test’s invention was scientifically significant – it was the first standardized bioassay to compare anabolic vs. androgenic potency side by side. Pharmaceutical labs in the 1960s extensively used the Hershberger test to screen hundreds of steroid analogues in the hunt for a “safe” anabolic steroid.
While some steroids (e.g. 19-nortestosterone derivatives like nandrolone) showed a somewhatbetter anabolic-to-androgenic profile than testosterone, none were completely tissue-selective. This highlighted the need for new approaches, setting the stage for selective androgen receptor modulators (SARMs)decades later.
Scientific usage: Beyond anabolic steroid development, the Hershberger test has become embedded in toxicology and endocrine research. It is now an internationally standardized assay (OECD Test Guideline 441) for detecting compounds with androgenic or anti-androgenic properties. In regulatory settings, it’s used to screen environmental chemicals for hormonal (endocrine-disrupting) activity that affects the androgen receptor.
In doping science, it helps evaluate if a substance has predominantly anabolic effects (desired for performance enhancement) with fewer androgenic effects (which cause side effects). Thus, the test’s role has expanded from drug development into broader pharmacological testing of any agents that influence androgen pathways.
Methodology of the Hershberger Test
The methodology of the Hershberger test is straightforward and reproducible, involving a short-term experiment in castrated male rodents to gauge anabolic response versus androgenic stimulation. The protocol consists of several key steps:
- Animal Model Preparation: Male rats (typically immature or young adult) are castrated (orchidectomized) to remove the source of endogenous testosterone. This causes their androgen-dependent tissues – such as the prostate gland, seminal vesicles, and the levator ani/bulbocavernosus (LABC) muscle – to regress in size due to lack of hormone stimulation. After castration, the rats are given time for these tissues to atrophy to a low baseline weight.
- Treatment Groups: The castrated rats are divided into groups and treated for a short period (usually 7–10 days, sometimes up to 2 weeks). One group receives the test compound (e.g. a potential SARM or steroid) at a defined dose each day. Other groups serve as controls – typically one group gets a vehicle (no hormone) to establish the baseline, and another may receive a known androgen like testosterone propionate as a positive control. In some protocols, a reference anabolic steroid dose is included to compare the test compound’s potency.
- Administration: The compound is administered via a consistent route (subcutaneous or oral, depending on the assay design). Over the treatment period, the compound (if it has androgenic/anabolic properties) will act on the rats’ androgen receptors in tissues. In a castrated rat, an anabolic agent can only exert effects by activating the androgen receptor, making this a clean system to test the compound’s intrinsic activity.
- Tissue Dissection and Measurement: At the end of the treatment, the rats are euthanized and dissected. Researchers carefully isolate and weigh several key androgen-sensitive tissues (the assay traditionally focuses on five organs):
- Levator ani muscle (and bulbocavernosus muscle): a pelvic skeletal muscle group very responsive to anabolic stimuli. An increase in levator ani weight indicates muscle growth (an anabolic effect).
- Ventral prostate and seminal vesicles (including coagulating glands): accessory sex glands that grow in response to androgens. Increases in their weight indicate androgenic effects on reproductive tissues.
- (Often measured are also Cowper’s glands and glans penis weights, as part of the extended OECD protocol, but the primary readouts are usually levator ani and ventral prostate.)
- Data Analysis: The weights of the tissues from treated rats are compared to those of control rats. A strong anabolic compound will significantly increase the levator ani muscle weight relative to the castrated controls. Androgenic activity is reflected by growth of the prostate and seminal vesicles. By examining the muscle-to-prostate weight ratio – sometimes called the Hershberger index – scientists quantify tissue selectivity. For example, if a drug caused a +40% increase in muscle mass but only a +10% increase in prostate weight, it demonstrates a high anabolic-to-androgenic ratio. This numeric ratio or differential response is crucial for evaluating whether a compound could be a selective anabolic agent.

Flowchart illustrating the Hershberger test procedure (scientific methodology). In this short-term animal model assay, castrated male rats are administered a test compound (or control) for about 1–2 weeks, then sacrificed to measure androgen-responsive tissues. Key organs like the levator ani muscle (for anabolic response) and the prostate/seminal vesicles (for androgenic effects) are weighed. By comparing the muscle weight gain to prostate growth, researchers determine the compound’s anabolic activity versus its androgenic impact (the androgenic–anabolic ratio), indicating tissue selectivity.
Quantifying anabolic vs. androgenic effects: The outcome of a Hershberger test is often summarized by how much the levator ani muscle grew relative to the accessory sex tissues. A highly anabolic-selective compound might restore muscle mass in castrated rats toward normal levels while barely affecting prostate weight. In contrast, a non-selective androgen (like testosterone) will increase both muscle and prostate significantly. This assay thus directly answers, “Does this compound build muscle without enlarging the prostate?” – the key question for separating anabolic activity from unwanted androgenic effects.
The simplicity of measuring tissue weights belies the assay’s power: it is a preclinical study that translates molecular action at the androgen receptor into tangible organ changes. Notably, the Hershberger test can also be adapted to detect anti-androgens by co-treating castrated rats with testosterone plus a candidate anti-androgen and seeing if the normal androgen-driven tissue growth is blocked.

Example results from a Hershberger assay comparing an experimental selective androgen receptor modulator (SARM) to testosterone in castrated rats. The bar graph shows levator ani muscle weight (anabolic target) and prostate weight (androgen-sensitive tissue) for each group.
The selective SARM dramatically increases muscle mass with only a minimal increase in prostate weight – indicating high anabolic activity with weak androgenic effects. In contrast, testosterone (a non-selective androgen) increases both muscle and prostate weights substantially. This illustrates how the Hershberger test differentiates an anabolic-selective compound from a traditional androgenic steroid.
Why the Hershberger Test is Essential in SARMs Research
The Hershberger test has proven essential in SARMs research as a practical in vivo assay to evaluate tissue selectivity. Selective androgen receptor modulators (SARMs) were designed to uncouple anabolic benefits from androgenic side effects, and the Hershberger assay is the go-to experiment to demonstrate this separation early in development. In fact, one can argue that modern SARMs stand on the shoulders of the Hershberger bioassay – it set the benchmark for what “selective” androgenic action means biologically.
When scientists began developing SARMs in the 1990s, they needed to show that these new compounds could build muscle without significantly stimulating prostate or other androgenic tissues. The Hershberger test provided exactly this readout. Early SARM candidates (nonsteroidal molecules) were first tested in castrated rats using the Hershberger assay to see if muscle weight gain outpaced prostate growth.
The first reports of nonsteroidal SARMs (circa 1998) showed increased levator ani muscle weight with negligible prostate enlargement – a breakthrough demonstration of anabolic selectivity in vivo. This result was revolutionary at the time: a compound acting on the androgen receptor that could preferentially produce an anabolic response (muscle growth) with reduced androgenic effect on the prostate.

From a drug development perspective, the Hershberger assay is a critical preclinical study for any prospective SARM:
- Proof of Concept: It provides tangible proof that a SARM is doing what it’s supposed to – augmenting muscle mass while sparing other tissues. A successful outcome (high muscle:prostate ratio) in this assay is often a gate for advancing a SARM candidate to more advanced models.
- Comparison to Traditional Steroids: The assay allows direct comparison of a SARM’s anabolic-androgenic profile against known anabolic steroids or androgens. For example, researchers can dose one group of rats with a SARM and another with testosterone (or another steroid) at an equi-anabolic dose, then compare prostate enlargement. A SARM that causes, say, 20% of the prostate growth that testosterone does for the same muscle gain is considered far more selective. This was observed with some early SARMs vs. dihydrotestosterone (DHT) in rat tests.
- Tissue Selectivity Index: The Hershberger readouts feed directly into calculating the androgenic-anabolic ratio. Compounds can be ranked by this ratio to pick the most tissue-selective agents for further development. SARMs by definition aim for a high anabolic (muscle) to androgenic (prostate/skin) ratio, and this assay quantifies that property.
- Guiding Medicinal Chemistry: Medicinal chemists use the assay results to tweak SARM structures. For instance, if a candidate still causes a bit too much prostate growth, chemists may modify the molecule and test analogues, iterating until the Hershberger test indicates minimal androgenicity. This practical feedback loop was inherited from anabolic steroid research in the 20th century.
In summary, the Hershberger test is tightly connected to SARMs research because it directly measures what SARMs were designed to achieve: muscle and bone growth without prostate or sebaceous gland stimulation. It bridges the gap between molecular design and physiological effect. Many landmark studies in the SARM field have cited Hershberger assay results to claim “tissue-selective activation of the androgen receptor” for their compounds.
Without this assay, proving the concept of a “selective androgen” would be far more difficult. Even today, any new SARM or androgen receptor agonist typically undergoes Hershberger testing as part of its characterization. The assay’s role in SARMs research is thus indispensable – it’s the filter that candidate molecules pass through to ensure they meet the primary criterion of selectivity before moving into long-term efficacy or toxicology studies.
Limitations and Criticisms of the Hershberger Test
Like any experimental model, the Hershberger test has its limitations and has faced criticisms, despite its broad utility. Some of the common methodological concerns include:
- Species and Physiology Differences: The assay uses rats as a proxy for human biology. Rats metabolize and respond to hormones somewhat differently than humans. For example, the rat levator ani muscle is not a major weight-bearing muscle in normal physiology (unlike human skeletal muscles used in weightlifting). A compound that is selective in rats might behave differently in primates. Thus, positive Hershberger results don’t guarantee efficacy or safety in humans – they are a first-pass filter. The relevance to human outcomes (like actual muscle function or prostate health) requires further validation in other models.
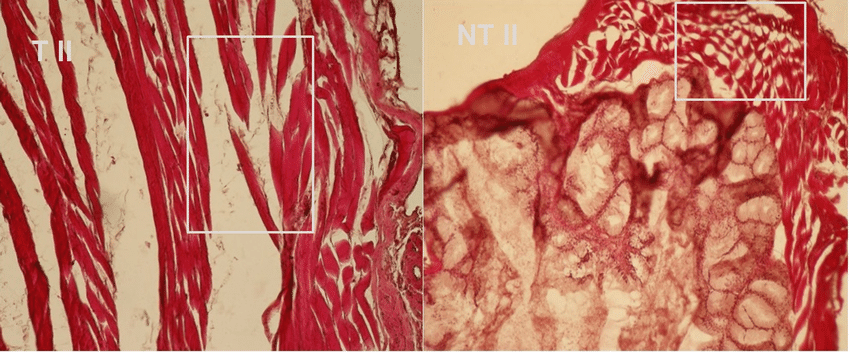
- Surrogate Endpoints: The test measures organ weight changes as a surrogate for functional effects. An increase in muscle wet weight is taken as a sign of anabolic effect, but it doesn’t directly measure muscle strength or performance. Similarly, a slight increase in prostate weight may not capture changes in histology or function. This means the assay could overlook qualitative differences (e.g. a compound might cause smaller prostate enlargement but induce disproportionate changes in prostate cell composition). Researchers mitigate this by complementing Hershberger results with other assessments (such as muscle fiber cross-sectional area, or gene expression profiles in tissues).
- Short-Term Assay: The Hershberger protocol is short (typically 1-2 weeks of treatment). It identifies acute anabolic and androgenic effects, but it might not reveal long-term side effects or compensatory mechanisms. A SARM could pass a 10-day Hershberger test with flying colors, yet over months of use it might gradually stimulate androgenic pathways (for instance via metabolite accumulation or receptor upregulation). Therefore, while a negative prostate effect in a short-term assay is encouraging, chronic studies are needed to ensure androgenic effects don’t appear with longer exposure.
- Variability and Reproducibility: Perhaps the most discussed criticism is assay variability across laboratories. Early on, different labs sometimes reported different absolute organ weight changes, raising concerns about reproducibility. Factors like rat strain, age at castration, diet, and even minor differences in dissection technique can impact organ weights. One analysis reported that results were only about 72% reproducible when the same 25 chemicals were tested in different labs, underscoring this variability. Such findings led some to suggest that in vitro assays might be better for consistent screening. However, extensive international validation efforts (led by the OECD) addressed these concerns. By standardizing the protocol, ensuring quality control in animal handling and measurements, and defining strict statistical criteria, researchers showed the Hershberger assay can be robust, reproducible, and transferable across labs. In fact, the OECD validation program found that when following the standardized guideline, multiple labs could consistently detect androgenic and anti-androgenic effects of both strong and weak test compounds. Today’s guidelines mandate including sufficient group sizes, proper controls, and calibrated techniques, which help minimize inter-lab differences.
- Ethical and Logistical Concerns: As an animal test, the Hershberger assay involves the use of a number of rats (including surgical castration and eventual sacrifice). This raises ethical considerations in line with the 3Rs (Replacement, Reduction, Refinement) of animal research. Efforts have been made to refine the assay – for instance, using the minimal number of animals to achieve statistical power, or exploring if certain endpoints can be measured via imaging rather than dissection. Additionally, the assay’s focus on male reproductive tissues means it doesn’t address effects in females or other hormonal systems. It’s a reductionist model concentrating on the androgen axis.
Need for validation: Given these limitations, scientists emphasize assay validation and reproducibility checks. The Hershberger test is often run alongside other assays (like in vitro AR binding/transcription assays and longer-term preclinical studies for muscle/bone) to build a weight of evidence. A compound that looks good in the Hershberger screen will still need to prove itself in broader pharmacological testing.
Assay controls are critical: including a known anabolic agent and a known antiandrogen in the experiment helps confirm that the assay is working as expected (positive and negative controls). Moreover, when used to screen environmental chemicals, positive Hershberger results are interpreted with caution – a slight increase in an organ’s weight might statistically signify androgenicity, but toxicologists consider whether it’s biologically meaningful or if there were confounding systemic toxicity that affected organ weight.
So the Hershberger assay, while essential and informative, is not infallible. Its critics point to the importance of not over-interpreting a single readout. The scientific community has responded by strengthening the test’s protocols and by always placing its results in context with other data. When properly executed, the Hershberger test remains a sensitive tool for what it was designed to do – detect androgenic/anabolic effects – but researchers must be mindful of its scope and ensure assay validation for reliable and reproducible outcomes.
FAQs
What exactly does the Hershberger test measure?
The Hershberger test measures the anabolic vs. androgenic effects of a compound in vivo by quantifying tissue growth in castrated male rats. In practical terms, it measures how much a test substance can stimulate muscle growth (notably the levator ani muscle) relative to androgenic growth of male sex organs (like the prostate gland and seminal vesicles).
An increase in levator ani muscle weight indicates anabolic activity, whereas increases in prostate/seminal vesicle weight indicate androgenic effects. By comparing these measurements, scientists determine if the compound preferentially builds muscle or also activates male reproductive tissues. The test thereby provides an androgenic–anabolic ratio or index for the substance being studied.
How is anabolic activity differentiated from androgenic effects?
Anabolic activity is differentiated from androgenic effects by examining which tissues grow and by how much during the Hershberger assay. After treating castrated rats with a compound, researchers look at muscle vs. organ responses: a selective anabolic agent will cause the levator ani muscle to increase in weight significantly, while causing little to no growth in androgen-sensitive organs (prostate and seminal vesicles).
This indicates the compound’s effects are mostly anabolic (muscle-building). On the other hand, if the compound also enlarges the prostate and related glands, those are androgenic effects (masculinizing side effects). By calculating the ratio of muscle growth to prostate growth (sometimes called the Hershberger index), scientists can clearly see the distinction.
For example, a drug that causes a 5-fold increase in muscle weight but only a 1.2-fold increase in prostate weight has a high anabolic-to-androgenic ratio, meaning its anabolic activity outweighs its androgenic impact. In essence, tissue selectivity is the key – the Hershberger test differentiates anabolic vs. androgenic by measuring target tissue selectivityof the compound’s action on the androgen receptor. This approach allows one to quantify how “selective” an androgenic compound is (i.e., does it mostly affect muscle, or does it equally affect all androgen-responsive tissues).
Conclusion
The Hershberger test has stood the test of time as a fundamental assay for evaluating anabolic activity in a scientific yet pragmatic way. By leveraging a simple animal model (castrated rats) and direct tissue measurements, it gives researchers a clear read on whether a compound can drive muscle growth without provoking excessive androgenic effects in other tissues.
This bioassay proved crucial in the development of anabolic steroids and later became even more valuable with the advent of selective androgen receptor modulators (SARMs), where the very goal is to maximize muscle and bone benefits while minimizing side effects. In the realm of SARMs research, the Hershberger assay provides early convincing evidence of a compound’s tissue selectivity – essentially asking, “Does this molecule act as a smart androgen?” and answering it with quantitative data.
In today’s pharmacological and toxicological evaluations, the Hershberger test is a validated, standardized tool, often used alongside molecular assays and clinical observations. Its scientific methodology exemplifies how understanding organ-specific responses can guide the design of safer and more effective anabolic therapies. While no single test is perfect, the Hershberger assay’s power lies in its clarity and focus on the androgenic–anabolic ratio, which remains a key concept for hormone modulators.
(Explore more in our other articles and comprehensive monographs on SARMs and anabolic research to delve deeper into this topic.)
References:
- Hershberger, L. G., Shipley, E. G., & Meyer, R. K. (1953). Myotrophic activity of 19-nortestosterone and other steroids determined by a modified levator ani muscle method. Proceedings of the Society for Experimental Biology and Medicine, 83(1), 175–180. https://doi.org/10.3181/00379727-83-20353
- Freyberger, A., Hartmann, E., & Krotlinger, F. (2005). Evaluation of the rodent Hershberger bioassay using three reference (anti)androgens. Arhiv za higijenu rada i toksikologiju, 56(2), 131–139. https://pubmed.ncbi.nlm.nih.gov/16882536/ScienceDirect+6OUCI+6cefic-lri.org+6
- Gao, W., Bohl, C. E., & Dalton, J. T. (2005). Nonsteroidal selective androgen receptor modulators (SARMs). Endocrinology, 146(4), 1473–1479. https://academic.oup.com/endo/article/145/12/5417/2499700Oxford Academic+1Oxford Academic+1
- Yamada, T., Kunimatsu, T., Miyata, K., Yabushita, S., Sukata, T., Kawamura, S., Seki, T., Okuno, Y., & Mikami, N. (2004). Enhanced rat Hershberger assay appears reliable for detection of not only (anti-)androgenic chemicals but also thyroid hormone modulators. Toxicological Sciences, 79(1), 64–74. https://pubmed.ncbi.nlm.nih.gov/14976338/Oxford Academic+4PubMed+4Wikipedia+4
- Browne, P., Kleinstreuer, N. C., Ceger, P., Deisenroth, C., Baker, N., Markey, K., Thomas, R. S., Judson, R. S., & Casey, W. (2018). Development of a curated Hershberger database. Reproductive Toxicology, 81, 259–271. https://www.sciencedirect.com/science/article/abs/pii/S089062381830145XPubMed Central+5PubMed+5ScienceDirect+5
- Organisation for Economic Co-operation and Development (OECD). (2009). Test No. 441: Hershberger Bioassay in Rats: A short-term screening assay for (anti)androgenic properties. OECD Guidelines for the Testing of Chemicals, Section 4. https://www.oecd.org/en/publications/2009/09/test-no-441-hershberger-bioassay-in-rats_g1ghbb57.html
About the author

Emiliano Ventura, PhD, Pharm.D.
Senior Scientist MetID & LC-MS
🧑🔬 Senior Scientist | 🧪 Bioanalytical Methods (LC-MS/MS) | 🔍 MetID (HRMS, Radiodetection) | 💊 Small Molecules 🧱 Peptides 🧬 Oligonucleotides | 🚴 Anti-Doping | 🌍 Life Sciences | 🌟 Science with Purpose
Find me on LinkedIn!
Read more
Explore the Historical Development of SARMs in our series of articles:
Early Anabolic Steroid Era (1940s–1960s):
1. How the First Anabolic Steroids Were Created
2. Why Early Anabolic Steroids Fell Short of Medical Expectations
3. Hershberger Test: How Scientists Measured Anabolic vs Androgenic Effects
Discovery of Hormone Receptors (1960s–1970s)
1. How Discovery of Androgen Receptors Changed Hormone Therapy
2. Role of Nonsteroidal Antiandrogens in SARMs Development
3. The Crucial Difference Between Steroidal and Nonsteroidal Androgens
Concept of Selective Receptor Modulators (1980s)
1. The Revolutionary Concept Behind SERMs
2. Why SERMs Became a Blueprint for SARMs
3. How Tissue Selectivity Became the Core of Hormonal Drug Development
The Birth of SARMs (1990s)
1. The Story Behind the First Nonsteroidal Androgen Receptor Agonists
2. James Dalton’s Groundbreaking Research on SARMs
3. Early SARMs Structures and Their Advantages Over Steroids
Rapid SARMs Expansion (2000s)
1. Early Human Trials of Ostarine: Promises and Results
2. Ligandrol (LGD-4033): A Powerful SARM in Clinical Research
3. Chemical Diversity of SARMs Developed in the 2000s
Clinical Trials and Regulatory Challenges (2010s)
1. Phase III Clinical Trials of Ostarine: Successes and Failures
2. Why Defining Clinical Endpoints Was Difficult for SARMs Trials
3. Regulatory Hurdles Facing SARMs Approval
SARMs in Sports and the Rise of Misuse
1. How SARMs Became the New Doping Trend in Sports
2. Why Athletes Were Attracted to SARMs Despite Risks
3. Health Consequences of Illegal SARMs Use: Documented Cases
SARMs Today and Future Perspectives (2020s)
1. Current SARMs Research: Where Do We Stand?
2. Potential Medical Applications of SARMs in the Next Decade
3. Emerging Compounds and Future Directions in SARMs Research
