Can SARMs really cause gynecomastia — or is it just bro science?
You’ve likely heard conflicting opinions: some say SARMs are “side-effect free,” while others claim they got puffy nipples after just a few weeks.
Let’s break down the actual science of how SARMs may (or may not) cause gyno, what’s driving the risk, and how researchers manage it in controlled settings.
🔑 Key Takeaways
- SARMs don’t convert to estrogen, but can still cause gyno indirectly through testosterone suppression.
- When testosterone drops, estrogen becomes functionally dominant, especially post-cycle — increasing the risk of gynecomastia.
- The most suppressive SARMs (e.g. RAD-140, LGD-4033, YK-11, S-23) carry the highest gyno risk, particularly at high doses or in extended cycles.
- Gyno symptoms include puffy nipples, tenderness, and sub-nipple lumps — often appearing after the cycle, during hormonal rebound.
- Gyno can usually be reversed if caught early with proper recovery protocols, but late-stage cases may require surgery.
- In legitimate research settings, gynecomastia is rare due to structured protocols, medical oversight, and mandatory post-trial recovery.
🚨 First, What Is Gyno?
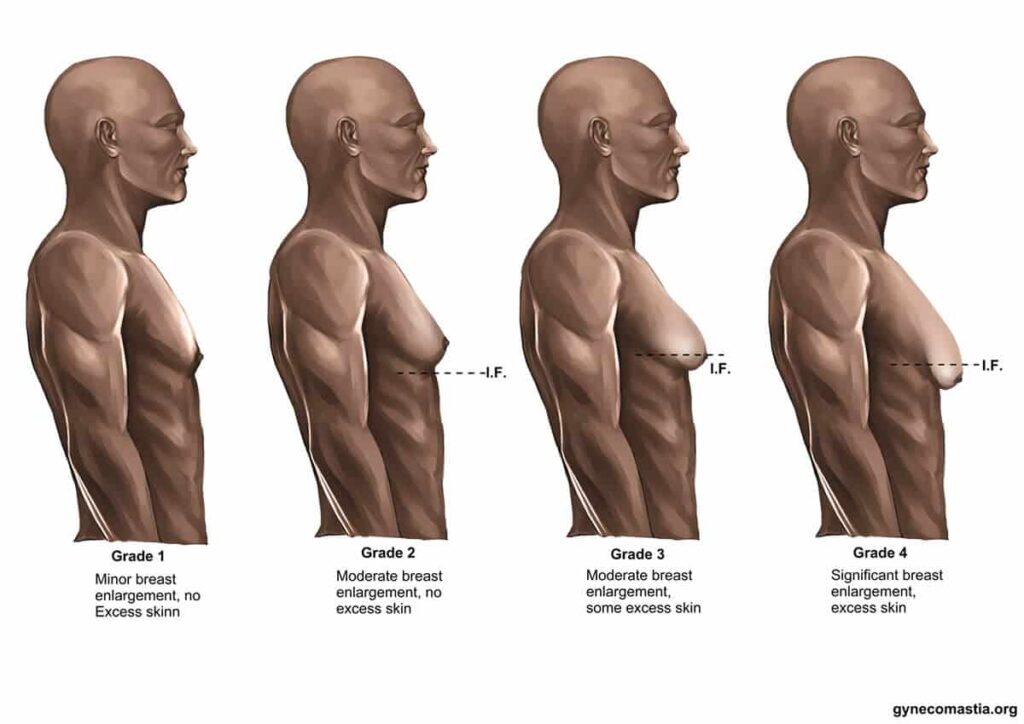
Gynecomastia — often shortened to gyno — is the benign enlargement of male breast tissue. It’s not fat; it’s glandular growth, often caused by hormonal imbalances, particularly increased estrogen activity relative to testosterone.
Symptoms include:
- Puffy or swollen nipples
- Tenderness or soreness
- Visible lumps under the nipple
Do SARMs Directly Increase Estrogen or Testosterone?
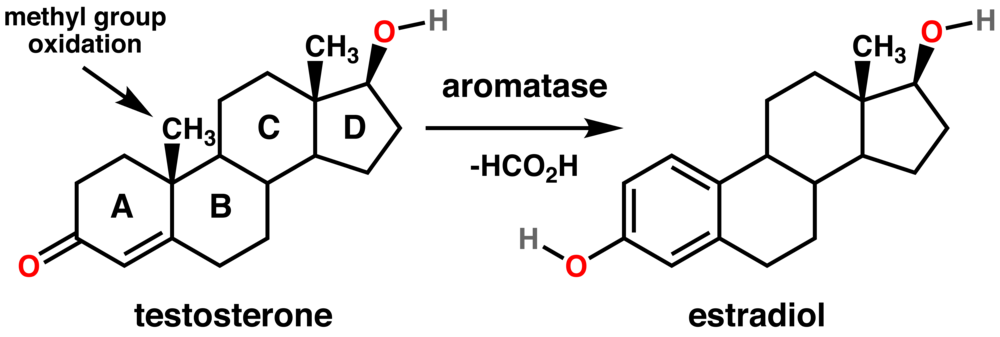
No. Most SARMs don’t aromatize into estrogen. This is one of their key differences from anabolic steroids.
However, SARMs can still indirectly cause hormonal imbalances that lead to gyno-like symptoms. Here’s how.
Further reading : Can SARMs raise testosterone?
⚙️ Mechanism: How SARMs Might Cause Gyno
1. Suppression of Natural Testosterone
Many SARMs suppress endogenous testosterone, even in relatively low doses. This can lead to:
- Reduced androgen:estrogen ratio
- Estrogen remaining unopposed
- Gyno symptoms emerging, especially post-cycle
- Testicular Atrophy
“In suppression scenarios, estrogen can become functionally dominant, even without increasing in absolute value.”
— European Journal of Endocrinology, 2019
2. Rebound Effect Post-Cycle
When you stop a SARM cycle, your testosterone is low, and estrogen may spike temporarily or remain elevated due to delayed recovery of the HPG axis. This estrogen rebound can promote glandular growth.
3. Individual Sensitivity
Some individuals are genetically predisposed to estrogenic symptoms. Even normal estrogen levels can trigger gyno in sensitive users.
“Gynecomastia may result from subtle shifts in the estrogen:androgen ratio, particularly in pubertal or predisposed males.”
— Mayo Clinic Proceedings, 2015
Which SARMs Have the Highest Gyno Risk?
| SARM | Aromatization | Suppression Level | Gyno Risk |
|---|---|---|---|
| RAD-140 | No | High | Moderate–High |
| LGD-4033 | No | High | High |
| Ostarine | No | Mild–Moderate | Low–Moderate |
| YK-11 | No | Very High | High |
| S-23 | No | Very High | High |
👉 Key Point: Risk is mostly dose-dependent and suppression-related, not due to estrogen conversion.
🧪 What Research Studies Say

Most clinical studies on SARMs (e.g., on Ostarine and LGD-4033) do not report gyno as a primary adverse event, but these are short-term studies, often under 12 weeks, with medical oversight and controlled PCT.
However, anecdotal data from self-administered cycles in the bodybuilding community shows a higher incidence of gynecomastia-like symptoms — especially without post-cycle therapy (PCT).
“While SARMs were developed to avoid androgenic side effects, suppression of the HPG axis remains a consistent finding in human trials.”
— JAMA Network Open, 2020
🔄 Can Gyno from SARMs Be Reversed?
Yes, in most cases — if caught early.
✅ Options include:
- Stopping the research trial
- Starting a proper doctor supervised PCT (e.g., Enclomiphene or Nolvadex under medical guidance)
- Using anti-estrogens (AIs or SERMs in research settings)
- In rare or late-stage cases: surgical removal may be needed
🛡️ How Researchers Avoid Gyno in SARMs Trials
In legitimate trials:
- Doses are kept low
- Suppression is monitored
- Subjects are withdrawn if adverse signs emerge
- PCT is administered as part of the study protocol
This underscores why SARMs aren’t legally approved for human use outside research — risks are real if not managed properly.
1. Use the Lowest Effective Dose
“Gyno risk rises sharply with supraphysiological doses.”
— Journal of Clinical Endocrinology & Metabolism, 2018
Minimising the dose helps maintain partial LH & HPG axis activity, reducing the chance of hormonal imbalance. In most human studies (e.g. Ostarine or LGD-4033), doses remain in the 1–3 mg/day range — far below what is often seen in unsupervised recreational use.
2. Keep Cycles Short
Clinical studies rarely exceed 6–12 weeks, which limits the cumulative suppression effect. Extended suppression increases the risk of estrogen dominance post-trial.
3. Monitor Hormonal Markers
Serious research trials include:
- Baseline and weekly bloodwork
- Tracking testosterone, LH, FSH, and estradiol (E2)
- Flagging significant changes for early intervention
“Frequent monitoring is critical to identify early endocrine disruptions.”
— Frontiers in Pharmacology, 2021
4. Include a Post-Cycle Recovery Protocol (PCT)
To restore hormonal balance, researchers may initiate post-cycle therapy (PCT) immediately after the trial ends. This typically includes:
- Selective Estrogen Receptor Modulators (SERMs) like tamoxifen (Nolvadex) or enclomiphene
- Duration: 2–4 weeks
- Goal: Stimulate natural LH/FSH production and testosterone recovery
This reduces estrogen:androgen imbalance, which is the primary driver of post-trial gyno onset.
5. Use Estrogen Modulators Only if Needed
In rare cases where estrogen symptoms appear during the trial (e.g. nipple sensitivity or swelling), researchers may deploy:
- Aromatase inhibitors (AIs): Anastrozole (Arimidex), Letrozole
- Low dose, short term to rebalance levels
- Used cautiously to avoid over-suppression of estrogen, which can lead to bone loss, lipid issues or blood pressure changes
6. Screen for Gyno-Prone Individuals
Some participants have a genetic or pubertal predisposition to gyno. Trials often screen for:
- History of pubertal gynecomastia
- Elevated SHBG or E2 baseline
- Obesity (which increases aromatase activity)
These subjects may be excluded or monitored more aggressively.
Summary: Gyno Prevention Protocol in Research Settings
| Strategy | Purpose |
|---|---|
| Low-dose SARM | Minimise suppression |
| Short cycle (≤8–12 weeks) | Reduce rebound risk |
| Bloodwork (T, LH, FSH, E2) | Detect early signs |
| SERM-based PCT | Support recovery post-cycle |
| Optional AI intervention | Manage acute estrogen symptoms |
| Participant screening | Identify high-risk individuals |
❓FAQ
Do all SARMs cause gyno?
No, but any SARM that suppresses testosterone can contribute to gyno symptoms, especially if PCT is skipped.
Can you get gyno from your first clinical trial?
Yes — especially with LGD-4033 or RAD-140. Sensitive users may notice early signs even in short cycles.
Will Nolvadex reverse gyno?
In research settings, SERMs like Nolvadex (tamoxifen) have been shown to reduce or reverse early gyno. Always consult medical professionals before use.
Is PCT always required after being part of a study?
If you use a suppressive SARM, then yes. Even Ostarine may require a mild PCT depending on dose/duration.
