Luteinising Hormone (LH) is a key player in the endocrine system — particularly when it comes to testosterone production, fertility, and the hormonal feedback loop that governs reproductive health in both men and women. Produced by the anterior pituitary gland, LH stimulates the Leydig cells in the testes to produce testosterone. Without LH, natural testosterone synthesis grinds to a halt.
For women, LH plays a central role in the menstrual cycle, triggering ovulation and supporting the production of progesterone.
How LH Works in the Body
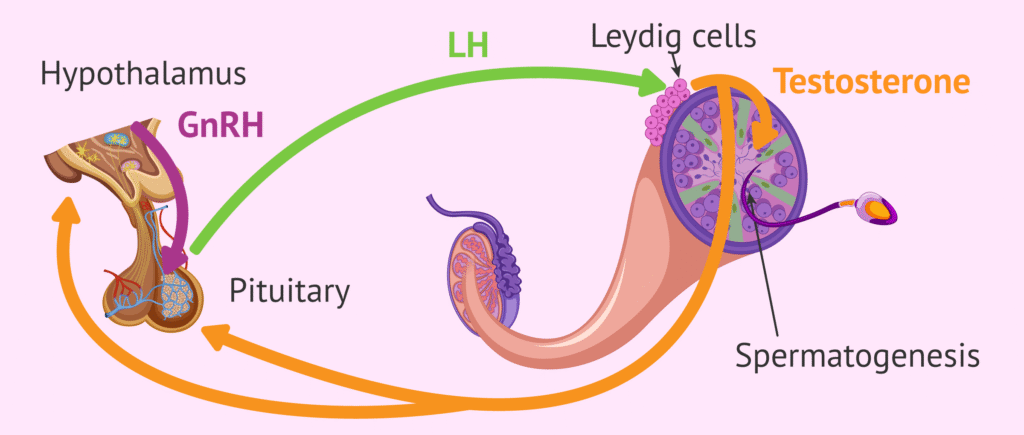
In men, LH acts like the “on switch” for testosterone. Here’s how the loop works:
- Hypothalamus releases GnRH (Gonadotropin-Releasing Hormone).
- GnRH stimulates the pituitary to release LH and FSH.
- LH stimulates Leydig cells in the testes to produce testosterone.
- Testosterone feeds back to the hypothalamus and pituitary to regulate LH production.
If testosterone levels drop (e.g. due to castration, suppression, or chemical intervention), the body usually increases LH secretion to compensate.
LH Suppression and SARMs: What’s the Connection?
SARMs (Selective Androgen Receptor Modulators) are often touted as a “safer” alternative to anabolic steroids. They work by binding to androgen receptors in muscle and bone tissue — promoting growth while theoretically sparing other organs. However, SARMs still activate negative feedback loops in the endocrine system.
“When SARMs are used at research-level dosages, they can suppress LH levels by tricking the body into thinking testosterone is already sufficient.”
— Endocrinology of the aging prostate, 2021
Here’s what typically happens:
- SARMs bind to androgen receptors and mimic the effects of testosterone.
- The body senses elevated androgen activity and reduces LH and FSH output.
- As a result, endogenous testosterone drops — sometimes dramatically.
- This is why post-cycle therapy (PCT) is often recommended after SARM studies.
Low LH = Low Testosterone = Risk of Hypogonadism
A sustained drop in LH can lead to hypogonadotropic hypogonadism, where the testicles no longer receive enough stimulation to produce testosterone. Symptoms may include:
- Low libido
- Erectile dysfunction
- Mood swings and fatigue
- Loss of muscle mass
- Infertility (due to reduced spermatogenesis)
- Testicular Atrophy
While SARMs are selective, they are not invisible to the endocrine system.
“Even supposedly non-suppressive SARMs like Ostarine have been observed to reduce LH and FSH levels in clinical models.”
— Journal of Clinical Endocrinology & Metabolism, 2020
Can LH Be Restored After SARMs?
Yes — but it depends on the individual, the SARM used, dosage, and duration. In most cases, LH rebounds naturally over several weeks once the SARM is discontinued. However, in more pronounced suppression cases, a PCT protocol using Clomiphene or Enclomiphene may be advised to stimulate LH production.
- Clomiphene works by blocking estrogen receptors in the hypothalamus, triggering increased GnRH and LH.
- Enclomiphene, the active isomer, is even more targeted and is used in clinical settings for male infertility, but has concerns about the effect of Enclomiphene on the Libido
Key Takeaways
- LH (Luteinising Hormone) is essential for natural testosterone production.
- SARMs can suppress LH, even though they are selective.
- Prolonged LH suppression may result in low testosterone and fertility issues.
- Post-cycle recovery — with or without PCT — may help reboot LH levels.
