Short answer: Yes — SARMs can cause acne, especially during or shortly after an authorised study. The risk and severity depend on the compound, dose, duration of use, and your individual hormonal sensitivity.
Acne isn’t just a cosmetic issue. It’s often a visible sign of hormonal imbalance — something worth taking seriously before you start any study.
Key Takeaways
- ✅ SARMs can cause acne — especially stronger ones like RAD-140 and S-23
- ✅ Acne risk increases with dosage, study length, stacking, and individual sensitivity
- ✅ Even “mild” SARMs like Ostarine remain capable of triggering skin issues
- ✅ Good hygiene + careful skin care + controlled dosing help minimize risk
- ⚠️ There is no guarantee against acne — treat the possibility as real, not optional
Why SARMs Might Trigger Acne: The Biological Mechanism
- SARMs bind to androgen receptors, simulating the effect of androgens (like testosterone).
- This boost in androgenic signaling — even if selective — can stimulate sebaceous glands (oil glands) in your skin.
- More sebum + androgen-driven follicle changes = blocked pores, inflammation, pustules.
- Additionally, some SARMs suppress the body’s natural testosterone production. After a study, hormonal fluctuations may further destabilize skin homeostasis, causing breakouts.
In medical terms, SARMs can disrupt your androgen–estrogen balance, which is a common trigger for acne — especially if your skin is already acne-prone.
To understand why SARMs can trigger acne, you need to look at how they influence your androgenic signaling pathway — the same system responsible for puberty, oil production, and hormonal balance in your skin.
Let’s break it down step by step.
1. SARMs Bind to Androgen Receptors
SARMs (Selective Androgen Receptor Modulators) are designed to mimic the effects of testosterone in muscle and bone — but they don’t completely avoid other tissues, like the skin and sebaceous glands.
- Your skin — particularly on the face, chest, and back — contains androgen receptors
- When SARMs bind to these receptors, they stimulate oil gland activity, just like testosterone and DHT (dihydrotestosterone)
Result:
➤ Increased sebum (oil) production → oilier skin
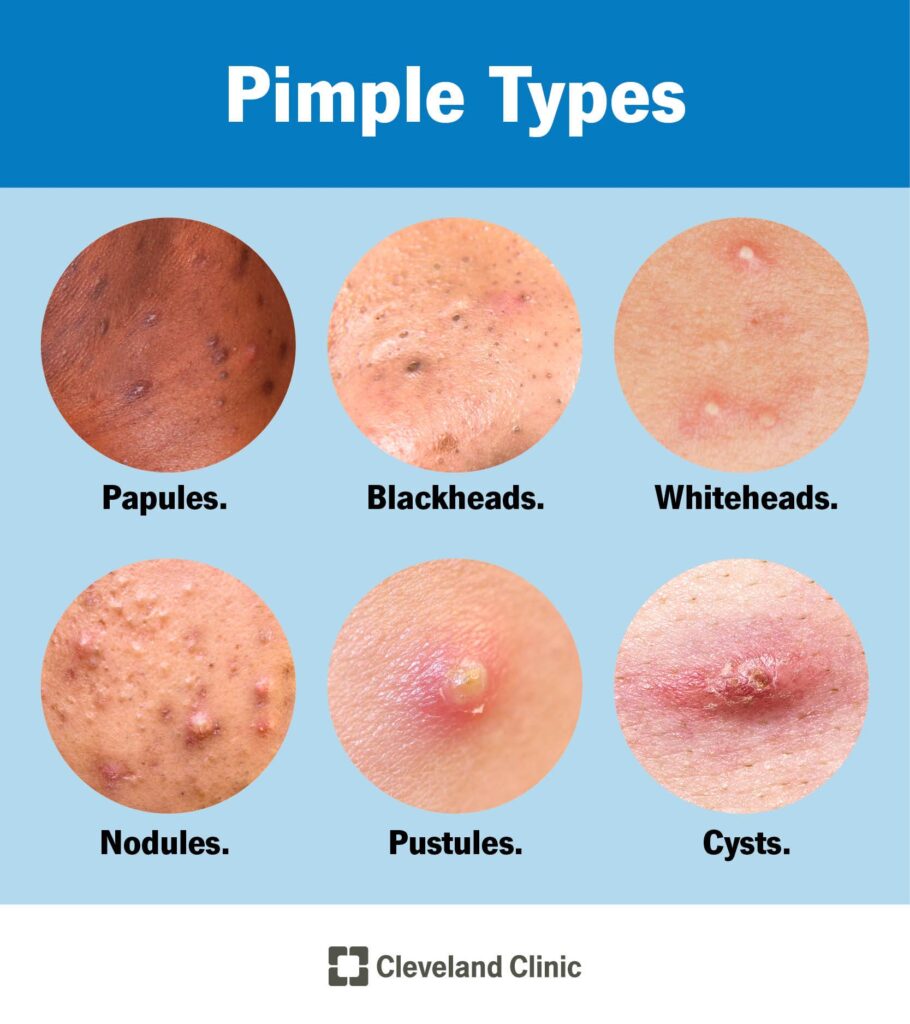
➤ More clogged pores → blackheads, whiteheads, and inflammatory acne
Learn more : Differences between Androgen Receptors and Peptides
2. Hormonal Imbalance and DHT Sensitivity
Although SARMs are often said to avoid DHT-related side effects, they can still trigger androgen-driven acne because of two things:
- Androgen Receptor Overstimulation: Some SARMs (like RAD-140 and S-23) have strong binding affinity, sending powerful signals even without converting to DHT
- Feedback Suppression: SARMs suppress LH and FSH → your natural testosterone drops
- This creates a hormonal rebound or instability, where estrogen may temporarily rise, and skin becomes more reactive
Result:
➤ Androgen-to-estrogen imbalance = one of the most common root causes of adult acne
Further reading : SERMS & the relation to SARMs side effects
3. Post-study Hormonal Fluctuation (“Rebound Acne”)
When you come off SARMs, your body needs time to restart its own hormone production. During this time:
- Testosterone is low
- Estrogen may spike relative to androgens
- DHT conversion can increase in some users due to enzymatic changes
- Sebaceous glands are still activated from the study, but now unregulated
This often leads to post-research study flare-ups, especially around:
- Chin and jawline (hormonal acne sites)
- Back and shoulders (classic “SARM backne”)
Further information on post research therapy using Enclomiphene here
4. Increased IGF-1 and Skin Cell Turnover

SARMs may also indirectly stimulate IGF-1 (insulin-like growth factor 1), which:
- Increases keratinocyte (skin cell) production
- Increases sebum output
- Contributes to blocked follicles and inflammation
This is a lesser-known acne pathway — but it mirrors what’s observed with anabolic steroids and growth hormone use.
Result:
➤ Overproduction of skin cells + excess oil = perfect storm for acne formation
Summary of the Acne Pathways Triggered by SARMs
| Mechanism | Effect |
|---|---|
| Androgen receptor activation in skin | Overstimulated sebaceous glands → more oil |
| Hormonal suppression & rebound | Testosterone crashes post-study→ estrogen imbalance |
| Sebum + clogged pores | Promotes whiteheads, blackheads, cystic acne |
| Elevated IGF-1 (indirect) | Increased skin cell turnover → blocked follicles |
| Increased inflammation | Greater skin sensitivity + redness, especially post-study |
Who’s Most at Risk?
You’re more likely to get acne from SARMs if you:
- Had acne during puberty
- Have oily skin or enlarged pores
- Are sensitive to hormonal fluctuations (especially DHT)
- Are running suppressive compounds (RAD-140, S-23)
- Stack SARMs without proper post-study recovery
- Neglect basic skin hygiene during study
Further reading : Are SARMs toxic?
Which SARMs Are Most Likely to Cause Acne?
Not all SARMs are equal when it comes to androgenic side effects and resultant acne risk:
🔴 High Acne Risk (Strong Androgenic Effect)
- RAD-140 (Testolone) — strong androgen receptor affinity + high potency
- S-23 — near-steroidal suppression, strong androgenic signalling
These tend to cause:
- Rapid oiliness
- Clogged pores
- Acne outbreaks — often within weeks
🟠 Moderate Acne Risk (Milder Androgenicity)
- LGD-4033 (Ligandrol) — suppresses hormones sharply, can trigger flares
- Ostarine (MK‑2866) — lower potency, but still capable of causing skin changes
🟡 Lower (But Not Zero) Risk
- SARMs with weaker androgenic activation — especially at low dose and short duration — may have milder impact
- Even then, people with genetic predisposition to acne remain at risk
Further reading : Side effects of Ostarine
Real‑World Patterns: What Users Report & Why Acne Persists
From anecdotal reports and early clinical observations:
- Acne often appears within 2–4 weeks of starting a SARM study
- Face and upper back are the most common sites (due to high density of sebaceous glands)
- Worse after higher doses, longer study, or stacking compounds
- Post-studyhormonal swings can cause late-onset acne as the body adjusts
Important: “Mild SARM” doesn’t mean “acne-free.” Skin reaction depends heavily on your individual hormone sensitivity and baseline skin health.
Can Acne from SARMs Be Controlled or Prevented for study patients?
Yes — but you need a proactive approach:
- Maintain rigid skin hygiene: gentle cleansing, avoid heavy oils, regular exfoliation
- Use non-comedogenic skincare products — especially moisturizers & sunscreens
- Monitor hormone fluctuations — some users respond better if they taper dose gradually
- Support skin health via nutrition: plenty of water, low-glycemic diet, antioxidants (vitamin C, zinc)
- Consider topical acne treatment (salicylic acid, benzoyl peroxide) — ideally after consulting a dermatologist
Bottom line: Acne from SARMs is manageable, but only if you treat it like a potential side effect and prepare accordingly.
What the Science Says — And What Remains Unclear
- There is no large-scale clinical trials on RAD140 or other SARMs explicitly linking SARMs with acne.
- But the androgenic mechanism is well-known to cause acne — extrapolating from steroids and endogenous androgen fluctuations gives valid reason for concern.
- Early user case reports often cite acne as a common complaint, though data are anecdotal.
⚠️ In short: absence of large studies ≠ absence of effect.
FAQ: SARMs & Acne
Do SARMs always cause acne?
No — but many users do experience breakouts, especially with high‑potency compounds or stacking.
Which SARM is least likely to cause acne?
Low‑dose Ostarine — but only if you’re not genetically acne-prone and maintain good skin hygiene.
Does acne go away after a SARM STUDY ends?
Often yes — but some users experience posts research breakouts due to hormonal rebound.
Can acne from SARMs be treated while part of an authorised study??
Yes — with non-comedogenic skincare routines and topical acne treatments; severe cases may require dermatological consultation.
Is acne a sign of serious damage?
Not usually — but it signals hormonal imbalance. Repeated hormonal fluctuations may have broader health consequences (e.g. endocrine disruption, fertility, heart health).
